Careers in Pathology in the UK: Training pathway for an IMG

Pathology is an intriguing speciality to pursue. Studying and looking into the cause of a disease, the pathology behind why something occurs, may very well be the things you are interested to know about. As it is a very diverse field there is no single entity or pathway titled “Pathology Training in the UK”, rather it is divided into some groups and subgroups which we will discuss from an international doctor’s point of view.
Related Subspecialties
Before we embark on the details of training in different branches of pathology in the UK, one thing needs to be known. Pathology is the bridge between medicine and science. So not only medical doctors but also clinical scientists can make a career in pathology in the UK.
For an international doctor wishing to make a career in pathology, they need to know about the following specialities & super specialities.
- Histopathology (cellular pathology)
- Chemical pathology (clinical biochemistry)
- Haematology
- Medical microbiology
- Medical Virology
- Clinical Immunology
- Forensic pathology
- Neuropathology
- Paediatric and perinatal pathology
- Oral & Maxillofacial pathology (for dental trainees)
You should know by now what a run-through and uncoupled speciality are. In the above list, histopathology and chemical pathology (without metabolic medicine) are run-though specialities. The core level of training before you can join other specific specialities can be any of the following:
- Internal Medicine training / ACCS-AM (acute medicine)
- Leads the way to join specialties like haematology, medical microbiology, virology, chemical pathology (with metabolic medicine), clinical immunology.
- Histopathology
- The initial stage of this training leads the way to join specialties like general histopathology, neuropathology, forensic pathology, paediatric and perinatal pathology.
There are other specific paths like from neurosurgery and neurology into neuropathology, but that’s too niche for a general discussion. If you are keen on a very specific path, the Royal College of Pathologists has everything laid out beautifully in their website.

Statistics related to training in pathology in the UK
The statistics below are for the Round 1 competition ratios for the CT1/ST1 specialities. We can clearly see a few important points:
- Histopathology had 109 posts in 2023 to recruit.
- Internal medicine training had 1670 posts in 2023.
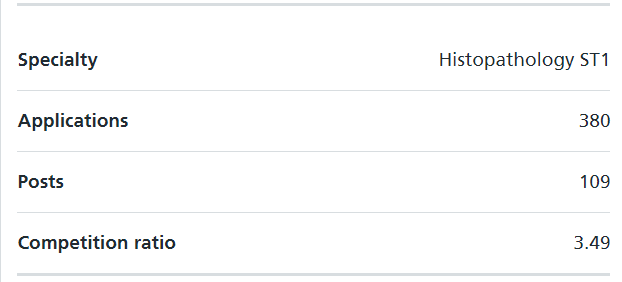
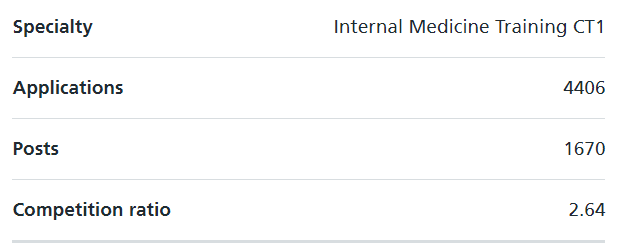
So, depending on which speciality you want to make a career in future, you have to find out whether to start with IMT/ACCS(AM) or Histopathology.
Prior to joining specialty training for an international doctor
If you are an International Medical Graduate (IMG), the very FIRST target is to obtain GMC registration with a license to practice. If you are unsure in what ways you can get that, please read How to get registered with the GMC UK.
The following discussion will require a basic understanding of how the training pathway for doctors is structured in the UK. This video will help:
The overview of career & training in pathology
We will go through the following related specialties and explain the training pathway in different careers in pathology in the UK from an international doctor’s perspective.
- Chemical pathology
- Histopathology
- Forensic pathology
- Cytopathology
- Neuropathology
- Paediatric & perinatal pathology
- Haematology
- Clinical Immunology
- Microbiology
- Virology
Please remember that the basic pathway to get into any training post in the UK includes:
- Getting GMC registration with a license to practice
- For any core level training, you need to have completed/signed off foundation competencies (CREST form) along with other entry criteria as per the person specifications of that post.
- For any specialty training, you MUST have completed the core level or have evidence that you have equivalent competencies of that (in the form of alternative core competence) along with other entry criteria (e.g. MRCP, MRCS etc completed) as per the person specifications of that post.
Just because you have passed MRCP (or any membership exams) doesn’t make you automatically eligible for higher specialty training. Each post has other entry criteria too. Please check your specialties’ person specifications here.
Chemical Pathology
Chemical pathology training in the UK can take the form of two roles:
- one as a chemical pathologist, and another
- as a chemical pathologist with a subspecialty interest in metabolic medicine.
If you are interested in pursuing pure chemical pathology, the path starts at ST1 and will take you five years to complete. This means that you will need GMC registration and a valid CREST form to apply. If you are interested in proceeding with an application for chemical pathology, it’s a good idea to check out the person specification for ST1 chemical pathology. You will need to complete both parts of FRCPath in Clinical Biochemistry as part of your training along with the Chemical Pathology Stage A exam.

If, however, you’re interested in going the route of metabolic medicine under the banner of chemical pathology, the process is a little different. After obtaining GMC registration, and getting your CREST form signed, you have the option to either enter Internal Medicine Training (IMT) or Acute Care Common Stem Acute Medicine (ACCS-AM) training. You will need to complete MRCP during this time.
The path to becoming a consultant in chemical pathology in the UK (metabolic medicine) will take you five and a half years of speciality training plus the two years of either IMT or ACCS-AM, and will also require you to clear the Chemical Pathology Stage A exam as well as FRCPath Parts 1 & 2 in Clinical Biochemistry.
Training to be a Chemical Pathologist
There are four stages of training that you need to be aware of that are demarcated by the following headings: A, B, C, and D.
- Stages A & B consist of your being introduced to the basic principles of chemical pathology with some practical experience.
- Stage C is the time where you will start stepping into the role of a consultant, and you will need to complete your exams during this period.
- Stage D will find you with minimal supervision, working independently towards your interests.
For more information related to chemical pathology, check out the curriculum as compiled by the Royal College of Pathologists.
Histopathology (Cellular pathology)
Histopathology (cellular pathology) training in the UK is a little more intricate than chemical pathology in that you can specialize in a couple of interesting fields such as forensic pathology, neuropathology, paediatric and perinatal pathology etc. You can also choose to just pursue general histopathology.
To start out, after getting GMC registration, you need to consider how you will go about getting your CREST form signed because histopathology starts at ST1 (a run-through speciality). It would be a good idea if you were interested in taking this path to become familiar with the person specification as laid out by the Royal College.
You’re looking at five years of training to become a histopathologist, and naturally, there are some exams to be concerned about along the way. You’ll need to complete the Histopathology Stage A exam as well as FRCPath Parts 1 & 2 in Histopathology. If you choose to specialize in something other than general histopathology, your route and exams change slightly.

The part 2 exam of your FRCPath would reflect the subspecialty you’re interested in training in i.e. forensics, pediatric pathology, etc. You’d also veer from general histopathology training at about the two to two and a half year mark to learn more about the subspecialty.
For example, if you want to become a forensic histopathologist, you’d need to clear the Histopathology Stage A exam, FRCPath Part 1 in Histopathology, and FRCPath Part 2 in Forensic Pathology. You’d also complete three years of training in forensic pathology after having done the first two years in histopathology.
Training to be a Histopathologist (forensic pathologist, paediatric pathologists or neuropathologist)
There are four stages of training:
- Stage A covers an introduction to surgical pathology, cytopathology, autopsy pathology and molecular pathology. Trainees can arrange a placement in paediatric pathology and neuropathology in either Stage A or Stage B.
- During stage B, you’ll broaden your experience and understanding of histopathology, and will need to demonstrate your ability to perform a number of tasks before moving on – including independently cutting up specimens, screening cervical samples and writing reports on specimens and frozen sections.
- During stages C and D you’ll have the opportunity to continue with histopathology, or specialise further in forensics, diagnostic neuropathology, paediatric and perinatal pathology or cytopathology. You’ll also be able to take on optional training in autopsies, cervical cytology and research methodology.
If you’re training full time, training to be a consultant histopathologist takes around five years. Once you have completed the first two years of histopathology training (that’s the core level training), you can decide to stay in general histopathology or move into one of the related sub-specialties – forensic histopathology, diagnostic neuropathology, paediatric and perinatal pathology or cytopathology.

Haematology
Haematology is an uncoupled speciality that consists of 2-3 years of core level training and then 4-5 years of higher speciality training. And the core part of this training pathway is either:
- Internal Medicine Training (2 years for this path)
- Acute care common stem – AM (Acute medicine) (3 years)
To join specialty training in haematology at the ST3 level you need to have the following things:
- Completed any of the core parts from the above OR evidence that you have completed the equivalent (either non-UK or in a non-training job)
- MRCP(UK) completed before joining in ST3 haematology
- At least 24 months of clinical work experience in medical specialties (of which at least 12 months must include the care of acute medical in-patients)
In your first year of specialty training in haematology, you will be given an introduction to laboratory aspects of haematology and, alongside this, the presentation and management of haematological disorders. After this, you’ll gain practical experience in blood transfusion, paediatric haematology, general haematology (such as the investigation of anaemia), haematological malignancy and haemostasis and thrombosis.
When on-call, you may be asked to respond to a haematological problem in any aspect of the subject – transfusion and coagulation problems are particularly common out-of-hours.
You will be supported at all times by a consultant and the responsibility you take will increase as you gain experience.
To complete your training, you’ll be required to pass the following.
- FRCPath Part 1 in Haematology – this aims to determine whether you have successfully acquired a core body of knowledge that will underpin your ability to practise in Haematology.
- FRCPath Part 2 in Haematology – this is designed to test your practical skills and understanding, and show that you can apply your expertise appropriately and safely.
Find more information here: Training in Haematology

Clinical Immunology
Like haematology, clinical immunology is also an uncoupled specialty that consists of 2-3 years of core level training and 4-5 years of higher specialty training. And the core part of this training pathway is either:
- Internal Medicine Training (2 years for this path)
- Acute care common stem – AM (Acute medicine) (3 years)
- Level 1 Paediatrics training ST1-2 (2 years)
To join specialty training in Immunology at ST3 level you need to have the following things:
- Completed any of the core level training listed above OR evidence that you have completed the equivalent (either non-UK or in a non-training job evidenced by an alternative core completion certificate)
- MRCP(UK) completed OR MRCPCH (UK) completed
- At least 24 months of clinical work experience in medical specialties (of which at least 12 months must include the care of acute medical in-patients) OR 24 months experience in paediatrics.
Higher specialty training in immunology will equip you to deliver a diagnostic immunology laboratory service, as you expand your knowledge to investigate and manage cases of congenital and acquired immunodeficiency disorders, autoimmune conditions (including rheumatic and allergic diseases).
You’ll learn the principles underlying organ and stem cell transplantation, and will be required to demonstrate key generic skills like communication and team-working, in accordance with Good Medical Practice.
To complete your training, you’ll be required to pass the following.
- FRCPath Part 1 in Immunology – this aims to determine whether you have successfully acquired a core body of knowledge that will underpin your ability to practise in Immunology.
- FRCPath Part 2 in Immunology – this is designed to test your practical skills and understanding, and show that you can apply your expertise appropriately and safely.
Reference: Training to be a clinical immunologist

Microbiology & Virology
Medical microbiology & virology are uncoupled specialties. The training structure for either of them in the UK has three parts.
- Core level training: Which can be any of the following-
- Internal Medicine Training (2 years for this path)
- Acute care common stem – AM (Acute medicine) (3 years)
- Combined Infection Training (CIT): for 2 years
- Higher Speciality Training: Further 2 years in microbiology or virology specifically.
To get into Combined Infection Training at ST3 level you need to have the following done:
- Completed any of the core level training listed above OR evidence that you have completed the equivalent (either non-UK or in a non-training job)
- MRCP(UK) completed before joining
- At least 24 months of clinical work experience in medical specialties (of which at least 12 months must include the care of acute medical in-patients).
For the first two years, in Combined Infection Training, it will include:
- six months of clinical microbiology training associated with a diagnostic laboratory
- six months of clinical infection consult duties
- six months of appropriate infection reed clinics where the major focus of the clinic is managing patients with infection. A combination of clinics could include HIV clinics, travel clinics or GUM clinics
- six months of clinical inpatient care of patients with infection.
And then microbiology or virology whichever path you choose, the next two years will be concentrated on those. While in training you have to complete the fellowship exam:
- FRCPath Part 1 in Infection – this aims to determine whether you have successfully acquired a core body of knowledge that will underpin your ability to practise in Virology/Medical Microbiology.
- FRCPath Part 2 in Virology/Medical Microbiology – this is designed to test your practical skills and understanding, and show that you can apply your expertise appropriately and safely.

To conclude, as we have discussed already there is no one single pathway called ‘pathology training in the UK’ – as diverse the specialty itself is, as diverse as the training in its different branches. As mentioned already, much of the content here is referenced from the official Royal College of Pathologists website and if you have any questions feel free to ask in the comments below.
Good Luck!

