Specialty Training in General Practice (GP) for IMGs

Unlike many countries, a doctor can NOT become a General Practitioner (GP) in the UK just with their primary medical qualification. The general practice (GP) training in the UK is a program that an overseas doctor (IMG)/UK graduates have to go through after completing the recruitment process. They then become eligible to register as a GP after successful completion of the training. The path may differ slightly for IMGs in the UK.
General Practice in the UK
GPs see patients of all ages, from newborn babies to the elderly. The ongoing relationship that GPs establish with their patients, and then the ability to offer continuity of care, is one of the most important and enjoyable aspects of the job.
GPs treat all common medical conditions and, if needed, they refer patients to hospitals and other medical services for urgent and specialist treatment. They focus on the health of the whole person, combining physical, psychological, and social aspects of care.
Career Opportunities of a GP
There are many options to develop your career within or alongside traditional general practice. Many GPs choose to work one or two sessions per week (i.e. half days) in a different role. It may be necessary in certain cases to gain additional qualifications (ex: sports medicine). In any case, it is important to keep up to date with relevant courses and training. So let’s talk about what you can do:
- Develop a special interest within GP work in areas such as adolescent health, child and adult safeguarding, diabetes, palliative medicine, minor surgical procedures, and musculoskeletal medicine.
- Become a clinical assistant to a consultant in a hospital outpatient clinic participating in research and development (R&D) for university departments, NHS research networks, and pharmaceutical companies.
- Teach medical students either at their university or within the GP practice (or both)
- Teach at postgraduate level – doctors in their second year of foundation training (F2) or those in a specialist GP training post (GP registrars)
- Become a GP appraiser with local colleagues
- Advise or serve on a Clinical Commissioning Group (CCG) or other health service bodies
- Examine for the Royal College of General Practitioners (RCGP)
- Work as a volunteer in the community and for charities
- Work in occupational medicine (focusing on health in the workplace) for the NHS, the military or private industry
- Work for a local or national sports team
- Work with special groups of people in prisons, the armed services and on ships
- Work as a police doctor and becoming a forensic medical examiner
- Work in medical journalism or medical politics
For further detailed discussion regarding where can your career as a GP can lead please read Explore General Practice as a career.
Let’s look at some statistics
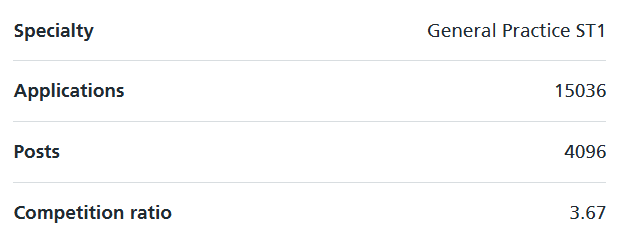
The UK has a shortage in GPs, which shows in the number of posts, but steadily over the past few years this has also led to an increase in applications.
Targeted Enhanced Recruitment Scheme
As we mentioned above regarding the shortage of GPs, many training sites now offer what is called a 'golden handshake' or an incentive to complete your training there. England has stated that they will not undertake TERS for the 2025/26 recruitment, but Scotland and Wales have not said anything regarding this.
Find out more about the TERS locations here.
How GP training is structured
As mentioned already, the actual General practice (GP) training for IMG/UK graduate is for 3 years, but you would have to have completed foundation training OR gain equivalent competencies before you can apply for GP training.
- Foundation Training
- General Practice Training
- GPs with Extended Roles (GPwER)
1. Foundation training
If you are a non-UK/EEA medical graduate, then you have three options:
- Obtain the equivalent of foundation training outside the UK
- Obtain the equivalent of foundation training inside the UK
- Getting into the foundation training by UKFPO.
You can get the certificate of readiness to enter specialty training (CREST) form signed by your overseas consultant if you had worked under them for at least three months after completion of your formal internship/house job and fulfill the points mentioned in the CREST form.
The same way, you can start working in the UK as a non-training doctor and after working under a consultant for at least three months, you can get those competencies signed off.
More information regarding joining UKFPO Foundation training – Internship and UKFPO can be found here.
Getting into UKFPO’s two-year foundation training is not applicable for those who have finished formal internship/house job following their graduation. If you hadn’t done your formal internship/house job after graduation for any reason (like taking USMLE, etc), you should do it before you think about moving to the UK. You will have to take PLAB/UKMLA both ways (UKFPO or home country’s internship), as you did not graduate from the UK/EEA.
2. General Practice Training
The training program lasts a minimum of 3 years where the rotations are primarily divided in two settings:
a. Hospital Setting
Based on the deanery and available rotations, a trainee is expected to spend 18-24 months rotating in different hospital specialties including (but not limited to) obstetrics and gynaecology, paediatrics, geriatric medicine, emergency medicine, or psychiatry, etc working at the level of core trainee (IMT1/ST1-3) in those specialties.
b. Approved General Practice Setting
The remaining 12-18 months will be spent on the general practice area which is approved for training purposes. This can be divided into 3 six months rotations where hospital rotations can happen in between.
c. MRCGP Exams
While in training, along with maintaining the portfolio to meet the training requirement a GP Trainee will also have to pass the MRCGP exam with two parts- Applied Knowledge Test (AKT) and Clinical Knowledge Assessment (CSA) in order to be eligible to get registered as a General Practitioner by GMC.
3. GPs with Extended Roles (GPwERs)
Previously known GPs with Specialist Interest (GPwSI). A GPwER is a GP who undertakes, in addition to their core general practice, a role that is beyond the scope of GP training and the MRCGP and requires further post-graduate training.
The extended role can cover areas that are non-clinical e.g. local medical committee, commissioning group or an interest in education (trainer, GP Tutor, appraiser). It could be clinical as well, for example (but not limited to):
- Dermatology
- COPD
- Cardiology
- Woman’s health
- Musculoskeletal healthcare/ sports injuries
- Reproductive health.
Please note that a “GP with a specialist interest in Dermatology” is not a “Dermatologist”. A GPwSI is primarily a generalist with some more specialist interest. A good specialist and a good GPwSI have many areas of similarity but have different skills to help in patient care. A GPwSI is bringing the wide spectrum of their clinical expertise and understanding of family and psychosocial issues to the clinical context.
Currently, there is no established accreditation as to how a GP can become GPwSI/GPwER. For now, It is advised by RCGP to follow the generic framework and contact providers and commissioners to understand local requirements until a proper framework is established.
What can an IMG (non-UK, non-EEA, without a settled visa) do to join GP training?
As mentioned already, there is no visa restriction (RLMT) to apply for general practice (GP) training for IMG in the UK. So if the following criteria are met, an IMG can go through the recruitment process and get into GP training.
- Be eligible for full registration with, and hold a current license to practice from, the GMC at the intended start date
- 12 months of medical experience after full GMC registration (or equivalent post licensing experience), and evidence to commence specialty training in the form of a Certificate of Readiness to Enter Specialty Training (CREST).
Please note that this 12 months of experience starts from your getting full registration in your country as well. And this is the minimum, there is no maximum experience limit like in some surgical specialties.
- Hold a current and in date valid driving license or provides an undertaking to provide alternative means of transport when providing emergency and domiciliary care to fulfill the requirements of the whole training program.
- Advanced Life Support Certificate from the Resuscitation Council UK or equivalent by intended start date.
Evidence of Foundation Training
Certificate of Readiness to Enter Specialty Training (CREST) will be accepted where the assessed post has been wholly undertaken in the 3½ years prior to the commencement of the training post to which the applicant is applying.
CREST can be signed off by your supervising UK consultant while you are doing a non-training job or by your consultant back at home while you were working as a fully registered doctor (provided you fulfilled the criteria mentioned in the form).
CREST form cannot be signed off for the duration of your work while you were in house-job/internship. You have to work as a fully registered doctor.
GP Training application process
It is a three-stage process.
- Application
- Assessment of eligibility (Stage 1)
- Long listing
- Multi Specialty Recruitment Assessment (MRSA): The MSRA is a computer-based assessment which forms the short-listing process (Stage 2). It consists of two papers:
- Clinical Paper,
- Professional dilemma paper (Situational Judgement test).
- Offers: There is a direct pathway to offers if you score 575 in MRSA. Otherwise, you will have to face an assessment in the selection center (Stage 3) where the applicants will go through simulated consultations and a written prioritization task.
- References
- Clearing
- Offers of employment and pre-employment checks.
For updated dates, always check the official recruitment website, National GP ST1 Recruitment site.
Ask a GP: Dr David Hopes
Dr. David Hopes works as a General Practice (GP) partner in England, and also is the Associate Dean of the Plymouth GP vocational training scheme (VTS). Aside from that, he works as an appraiser for other GPs and an educational supervisor for those in training.
He sat down with us to talk about life as a GP along with why he became one. Dr. Hope offers priceless advice regarding the pathway, gives his thoughts on how one could prepare to enter GP training, discusses the difference between a salaried GP and a GP partner, and some of the challenges he faced as a GP.
That’s all about GP training in the UK. If you are interested in other specialties check our blogroll and look for “Specialty training in the UK” tab under Professional Development.

